Your face says more about your health than you might think. A tight jaw after a long workday, a dull ache near your temple, or that clicking sound every time you yawn are not just random quirks. They are signals from your body that something deeper may be going on.
This guide breaks down what orofacial pain symptoms mean, how to tell if the discomfort is temporary or a sign to visit your dentist, and simple ways to find lasting relief. The goal is not to overwhelm you with medical terms but to help you understand your body’s cues before the pain becomes part of your routine.
At Elizabeth L. Wakim DDS, we take a comprehensive approach to diagnosing and managing orofacial pain. Our team combines advanced digital imaging, gentle diagnostic techniques, and personalized treatment plans to identify the root cause of discomfort and restore long-term comfort. Whether your symptoms are new or ongoing, we help you find relief that lasts.
What Does Orofacial Pain Actually Mean?
Orofacial pain refers to any discomfort felt in the face, mouth, or jaw. It can affect the muscles you use to chew, the joints that help you open your mouth, or the nerves that carry signals between your teeth and brain. While it may sound like a single condition, it is actually a broad term that includes many possible causes such as jaw disorders, nerve irritation, or muscle strain.
Some people describe it as a dull ache that lingers and worsens with stress or movement. Others feel sharp or burning pain that seems to appear without warning. Because the mouth and face share a complex network of muscles, joints, and nerves, it can be difficult to pinpoint the true source without a professional evaluation.
Dentists who specialize in orofacial pain can identify subtle patterns, such as nighttime clenching, uneven bite pressure, or nerve-related sensitivity. Understanding where your pain starts and what triggers it is the first step toward long-term relief and healthier function.
Recognizing the Symptoms You Might Be Ignoring
Orofacial pain can appear in different ways, and many people mistake the early signs for simple stress or fatigue. Knowing what to look for can help you catch potential problems early.
Here are five common symptoms worth paying attention to:
- Jaw stiffness or soreness that feels worse in the morning or after long hours at your desk
- A dull ache or pressure that spreads from the jaw to the temples, ears, or neck
- Clicking or popping sounds when you open or close your mouth
- Headaches or facial tension that seem to appear after chewing, talking, or clenching
- Sharp or one-sided pain that makes it uncomfortable to eat, yawn, or smile
Even mild discomfort can interfere with your daily routine if left untreated. If these symptoms keep returning or seem to be getting worse, schedule a dental evaluation to identify the cause and prevent further strain on your jaw and facial muscles.
What’s Causing It? The Usual Suspects (and the Hidden Ones)
Orofacial pain is not one single condition. It can have several overlapping causes, from muscle tension to nerve irritation. Because your mouth, jaw, and face work together for chewing, speaking, and expression, pain in one area often affects another.
Temporomandibular Joint (TMJ) Disorders
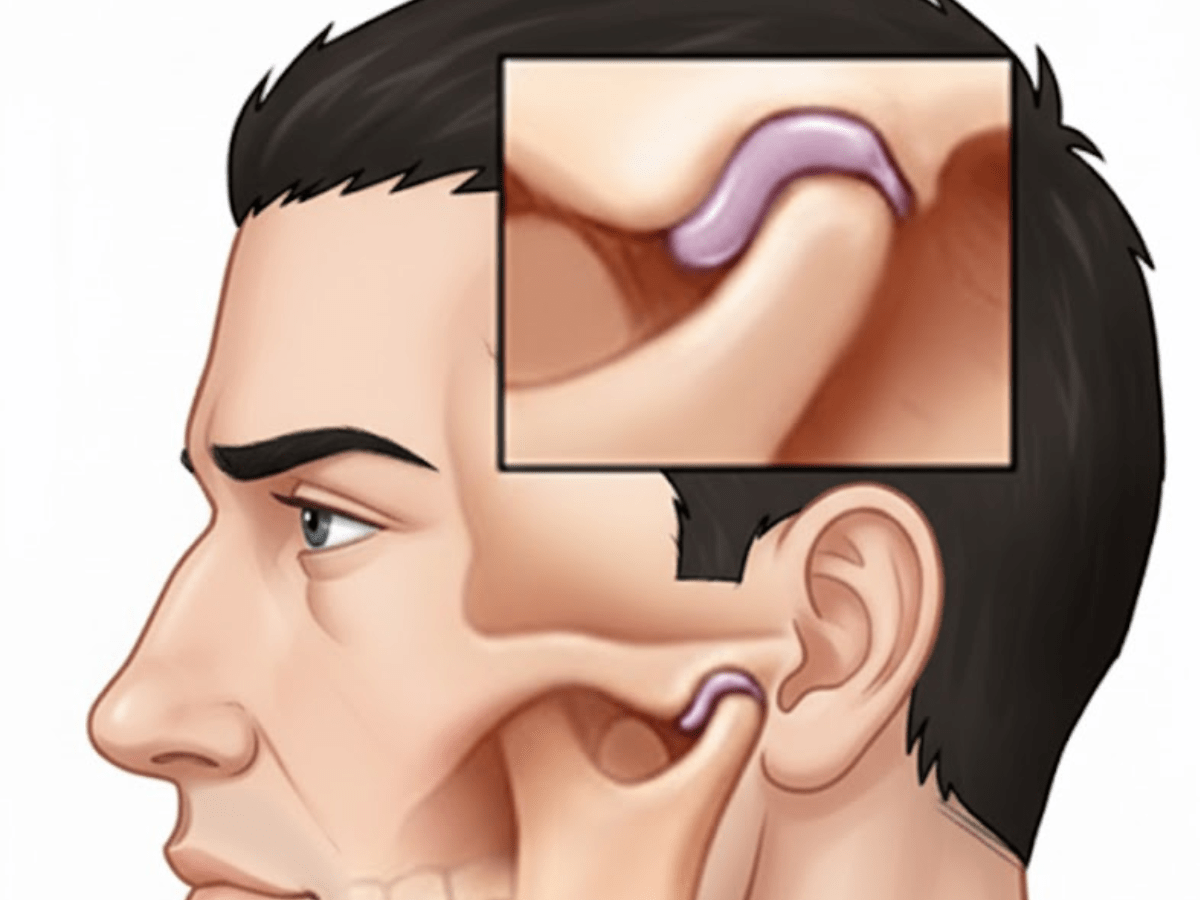
About 5 to 12 percent of adults experience symptoms of temporomandibular joint (TMJ) disorders, making TMJ problems one of the leading causes of persistent orofacial pain. The TMJ connects your jaw to your skull and allows smooth movement for speaking, eating, and smiling. When these joints become strained from stress, poor posture, or injury, the surrounding muscles and ligaments can tighten, leading to stiffness in the neck region and jaw discomfort.
Muscle Tension and Clenching
Tight facial and neck muscles can lead to myofascial pain, which creates aching, throbbing, or stabbing sensations that radiate through the head and neck. This type of pain may worsen with stress, poor posture. The tension can trigger secondary issues like headache disorders, jaw discomfort, or facial tightness that make it difficult to relax.
Teeth Grinding (Bruxism)
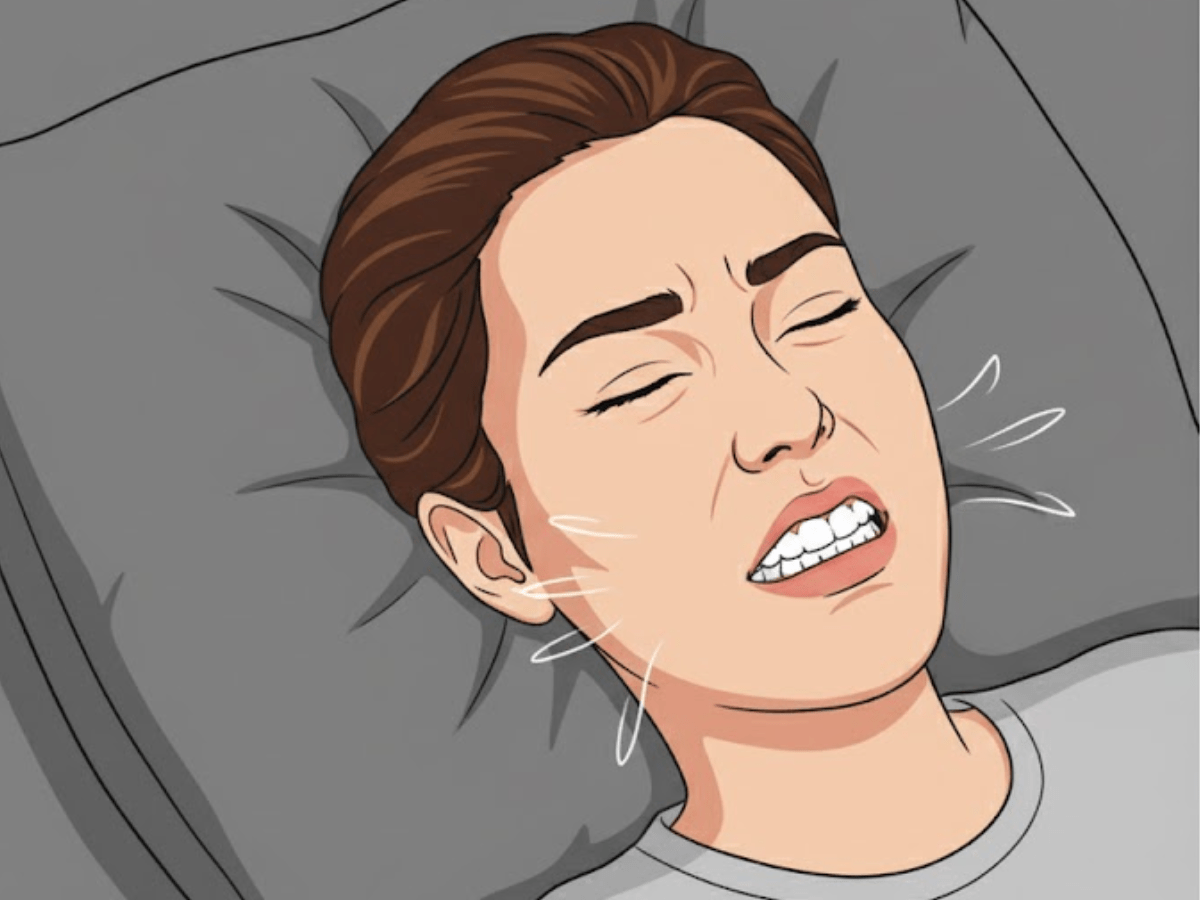
Studies show a global prevalence of about 22 percent for combined sleep and awake bruxism, making teeth grinding one of the most common habits linked to facial and jaw pain. Grinding or clenching the teeth, especially during sleep, can irritate the jaw joints, wear down enamel, and create pressure that radiates to the temples or facial area. Over time, this repetitive movement may lead to temporomandibular disorders and even nerve-related conditions that tend to worsen without proper treatment.
Dental Problems
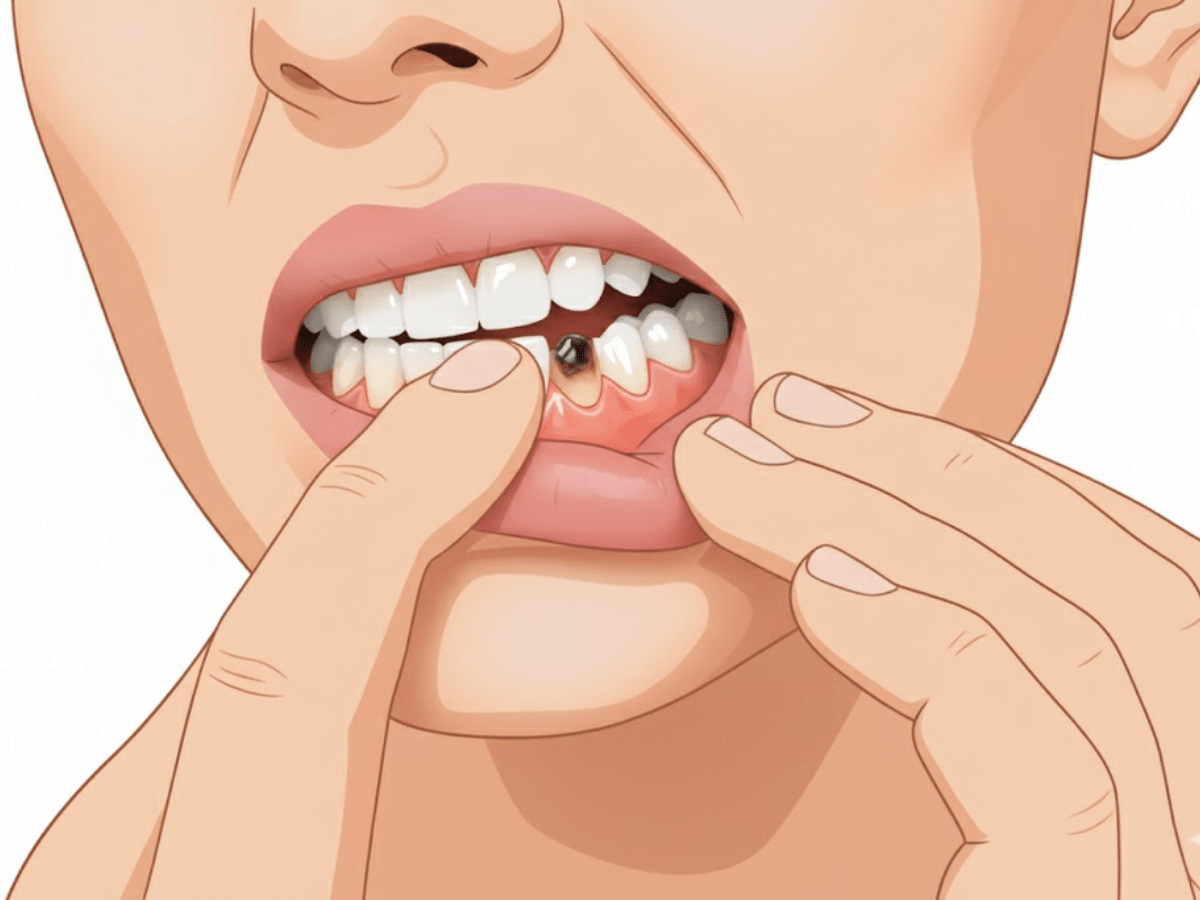
Issues such as tooth decay, gum disease, root canals, or fungal infections can produce pain that feels like it originates in the jaw or face. Because the nerves that run through the head and neck region are highly interconnected, dental pain can mimic other facial pains or nerve pain.
Nerve-Related Pain

Neuropathic pain affects an estimated 3 to 17 percent of the general population, making it a significant contributor to chronic facial discomfort. When the peripheral or cranial nerves are affected, pain may appear as burning, tingling, or electrical sensations across the facial area. Conditions such as neuropathic pain, atypical facial pain, or burning mouth syndrome can result from nerve damage, systemic diseases, or neurovascular disorders, often leading to persistent discomfort that requires professional evaluation.
Other Contributing Factors
Certain systemic diseases, sleep-related breathing disorders, or obstructive sleep apnea can worsen pain disorders and disrupt normal healing. Sinus pressure, nasal congestion, or involuntary movements of the jaw muscles can also amplify pain signals. In some cases, trauma from automobile accidents or strain from prolonged posture may trigger rapid-onset pain in the head and neck region.
Understanding these causes helps your dentist identify where the pain starts and design a plan that addresses both the symptoms and the root problem.
How Dentists and Specialists Diagnose Orofacial Pain
Because orofacial pain can come from many different sources, diagnosing it requires careful evaluation. A dentist trained in orofacial pain looks beyond the surface to uncover the patterns and triggers behind your symptoms.
1. Comprehensive Health and Pain History
The first step is a detailed conversation about your symptoms. Your dentist may ask when the pain started, how often it occurs, what triggers it, and how intense it feels. They will also review your medical and dental history to rule out related conditions such as sinus issues, nerve disorders, or past jaw injuries.
2. Physical and Functional Examination
Your dentist will gently examine your face, jaw, and neck to check for muscle tenderness, joint clicking, or restricted movement. They may observe how your bite aligns and how your jaw moves when opening and closing. This step helps pinpoint whether the pain comes from the muscles, joints, or teeth.
3. Imaging and Diagnostic Tools
If the source of pain is unclear, advanced imaging such as panoramic X-rays, cone-beam CT scans, or digital 3D imaging can reveal hidden dental or joint issues. These technologies allow your dentist to see inflammation, joint misalignment, or nerve compression that may not appear during a regular exam.
4. Rule-Out Approach
Because orofacial pain can mimic other conditions, dentists often work by elimination. They may collaborate with specialists in neurology, ENT, or pain management to exclude sinus infections, migraines, or neuralgia. This approach ensures that treatment targets the true source of pain rather than just the symptoms.
5. Personalized Diagnosis and Care Plan
Once the cause is identified, your dentist will create a care plan designed for your specific condition. This may include muscle therapy, oral appliances, posture correction, or dental adjustments. In some cases, a multidisciplinary approach provides the best long-term relief.
Accurate diagnosis is the key to lasting comfort. The goal is not just to relieve pain for the moment but to understand the underlying patterns that keep it coming back.
Treatment and Relief: From Simple Fixes to Advanced Care
Orofacial pain treatment depends on what is causing the discomfort. Some cases improve with small lifestyle changes, while others may need targeted dental or medical care. The goal is to relieve pain, restore movement, and prevent future flare-ups.
Here are the most common treatment approaches:
- Self-care and home relief. Applying warm compresses, practicing gentle jaw stretches, and avoiding hard or chewy foods can reduce strain on the jaw muscles. Maintaining good posture and managing stress also help ease tension over time.
- Oral appliances and night guards. Custom-made dental guards prevent teeth grinding and reduce joint pressure during sleep. They protect enamel, relax facial muscles, and promote better jaw alignment.
- Medication support. Dentists may recommend anti-inflammatory medication, muscle relaxants, or short-term pain relievers to control inflammation and improve comfort.
- Physical therapy and relaxation techniques. Jaw exercises, massage, or physical therapy can help strengthen muscles and restore normal movement. Breathing exercises, meditation, or stress management programs may also help break the pain-stress cycle.
- Dental or corrective treatment. In some cases, adjusting the bite, replacing damaged restorations, or treating underlying dental infections can eliminate the source of pain.
- Advanced options. For chronic or nerve-related pain, specialists may use targeted therapies such as injections, nerve blocks, or specialized pain management programs.
Preventing recurrence is just as important as treatment. Small changes in posture, sleep habits, and daily routines can help keep the jaw relaxed and functioning properly long after the pain subsides.
Everyday Habits to Protect Your Jaw and Face
Long hours on screens, high stress, and fast-paced routines can all take a toll on your jaw and facial muscles. Small adjustments in daily habits can make a noticeable difference in preventing orofacial pain and keeping your smile relaxed and healthy.
Here are simple ways to protect your jaw and facial muscles:
- Practice mindful posture: Keep your screen at eye level and your chin parallel to the floor. Good posture supports your jaw and neck muscles and helps prevent strain that can trigger tmj problems or jaw pain.
- Limit phone scrolling positions: Looking down for long periods can stress the neck and jaw. Holding your phone higher or taking quick stretch breaks helps keep the head and neck aligned and eases tension in the peripheral nerve pathways.
- Relax your bite: When resting, keep your lips closed but your teeth slightly apart. This prevents clenching and reduces pressure on the joints and surrounding muscles. People who grind or clench during sleep (sleep bruxism) often benefit from gentle jaw exercises or professional guidance to treat facial pain.
- Sleep smarter: Lying on your back with a supportive pillow allows your jaw to rest in a neutral position. Side sleeping or pressing your mouth wide against the pillow can strain the joints and muscles over time. Consistent sleep patterns also lower stress and may reduce sleep disorders linked to jaw discomfort.
- Manage daily stress: Stress often shows up first in the jaw or temples. Gentle massage, breathing exercises, or stretching your neck can help relieve tension and promote temporary pain relief.
Your jaw works hard every day. By giving it a little attention and care, you can prevent unnecessary pain, improve comfort, and protect your overall oral health.
Finding Relief and Lasting Comfort
Orofacial pain is more common than many people realize. It can interfere with how you eat, speak, and rest, but it is not something you have to live with. When diagnosed early, most cases can be managed with targeted dental care and simple lifestyle adjustments that protect your long-term comfort.
At Elizabeth L. Wakim DDS, we take a thorough and compassionate approach to identifying the source of jaw and facial pain. Using advanced imaging, gentle diagnostics, and personalized treatment plans, our team helps patients find relief that lasts while improving overall oral health and function.
Our team is committed to protecting your smile with gentle, personalized care. If you’re experiencing jaw tension, facial soreness, or pain that makes chewing uncomfortable, we’re here to help. Contact our Pennsylvania office at (724) 558-8222 or use our contact form to schedule a visit and get the expert support you need for a healthier, more comfortable smile.

