That throbbing toothache you’ve been brushing off? It could be more than a cavity. Dental abscesses don’t always start with dramatic swelling or obvious pain but when left untreated, they can turn into a serious medical concern fast.
At Elizabeth L. Wakim DDS, we believe in staying ahead of dental problems with early intervention and personalized care. If something feels off with your tooth, don’t wait it out.
Recognizing the early warning signs before they escalate is key to protecting not just your smile but your wellbeing. Let’s break down the symptoms of an abscessed tooth, some are more subtle than you might think, but all are worth paying attention to.
What Is an Abscessed Tooth?
Roughly 200,000 Americans visit the ER each year for dental abscesses, making up about 25% of all oral health-related emergencies. These painful infections often begin with untreated tooth decay, a cracked tooth, or gum disease, giving bacteria a path to the tooth’s soft inner pulp or surrounding gum tissue.
Once inside, bacteria multiply and cause a buildup of pus. This creates pressure, swelling, and sometimes intense pain. Left untreated, the infection can spread to nearby teeth, bone, and even other parts of the body.
There are two main types of dental abscesses:
- Periapical abscess: Forms at the tip of the tooth root, often from deep cavities or trauma.
- Periodontal abscess: Develops in the gums next to the tooth, typically due to advanced gum disease.
Both conditions need prompt dental care to avoid serious complications and in many cases, a regular dental checkup can detect these issues early enough to save your tooth.
What Are the Symptoms of an Abscessed Tooth?

Some dental issues can wait. This isn’t one of them. Tooth abscesses account for more than a quarter of dental-related ER visits in the U.S., second only to pain from untreated cavities. What often begins as mild discomfort can escalate fast especially if the infection spreads beyond the affected tooth. Ignoring the signs can lead to serious complications.
Here are the red flags to watch for:
- Throbbing pain that won’t go away: Persistent, sharp, or throbbing pain is one of the most common signs. It might radiate to your jaw, neck, or ear, especially on the side of the infected tooth.
- Swollen gums or face: Swelling around the gum line or cheek is your body’s response to the pocket of pus that forms when bacteria invade the tooth. In advanced cases, swelling may reach your face or lower jaw.
- Tooth sensitivity: If you’re suddenly flinching when sipping hot or cold food, or biting down causes pain, your tooth could be under attack. This is often a sign of exposed nerves or inflamed dental pulp.
- Unpleasant taste or odor: A bitter taste in your mouth or persistent bad breath may indicate that the abscess ruptures and is draining. That doesn’t mean the infection is gone, it still needs professional care.
- Fever or fatigue: Systemic symptoms like a fever, swollen lymph nodes, or feeling unusually tired may signal that the bacterial infection is spreading. Those with a weakened immune system are especially at risk.
Even if the pain fades, the danger hasn’t. Only a dentist can diagnose an abscessed tooth properly, prescribe antibiotics if needed, and restore your oral health the same way this post explains why you shouldn’t ignore a persistent toothache.
Underlying Causes & Risk Factors
With dental infections affecting an estimated 3.7 billion people worldwide, it’s clear that oral health concerns are incredibly common. A tooth abscess doesn’t appear overnight, it usually stems from untreated problems that allow bacteria to invade the inner layers of the tooth, including the pulp, nerves, and blood vessels.
Here’s what commonly causes an abscess:
- Untreated tooth decay: Cavities that aren’t addressed can deepen over time, giving bacteria a direct path to the inner tooth and leading to a periapical tooth abscess.
- Cracked or chipped teeth: Even small fractures can expose the tooth’s interior, creating an entry point for bacteria and increasing the risk of infection.
- Gum disease (periodontal disease): Advanced gum disease can cause pockets between the teeth and gums, where bacteria thrive and eventually affect the tooth’s root.
- Poor dental habits: Infrequent brushing, not flossing, or skipping regular dental checkups can allow plaque and decay to go unnoticed and untreated.
- Weakened immune system: Conditions like diabetes, autoimmune disorders, or treatments like chemotherapy may reduce your body’s ability to fight bacterial infections, making you more vulnerable to abscesses.
Recognizing these risk factors early can help you and your dental team act before a minor issue becomes a painful emergency especially when preventative dentistry empowers you to avoid costly treatments later on.
What to Expect: Diagnosis & Treatment Overview
When a tooth abscess starts, it often feels like a dull ache but without proper care, it can quickly escalate into a painful dental condition. Left untreated, a tooth infection can spread beyond the affected tooth, damaging surrounding connective tissue, bone, and even leading to life-threatening complications.
Here’s what to expect during diagnosis and treatment:
Dental Exam and Imaging

To confirm the problem, your dentist will examine the area and ask about your tooth pain, including any sensitivity to hot or cold temperatures, swelling, or difficulty chewing. They may also look for a swollen bump or signs of swelling in your face. A dental X-ray helps show if the abscess is a pocket of pus near the root or in the upper or lower jaw.
Drainage and Relief

If the infection is severe or the abscess ruptures, your dentist may need to drain it. This sometimes involves placing a small rubber drain to help remove pus and reduce pressure. Rinsing with warm saltwater can also support the healing process.
Root Canal Treatment
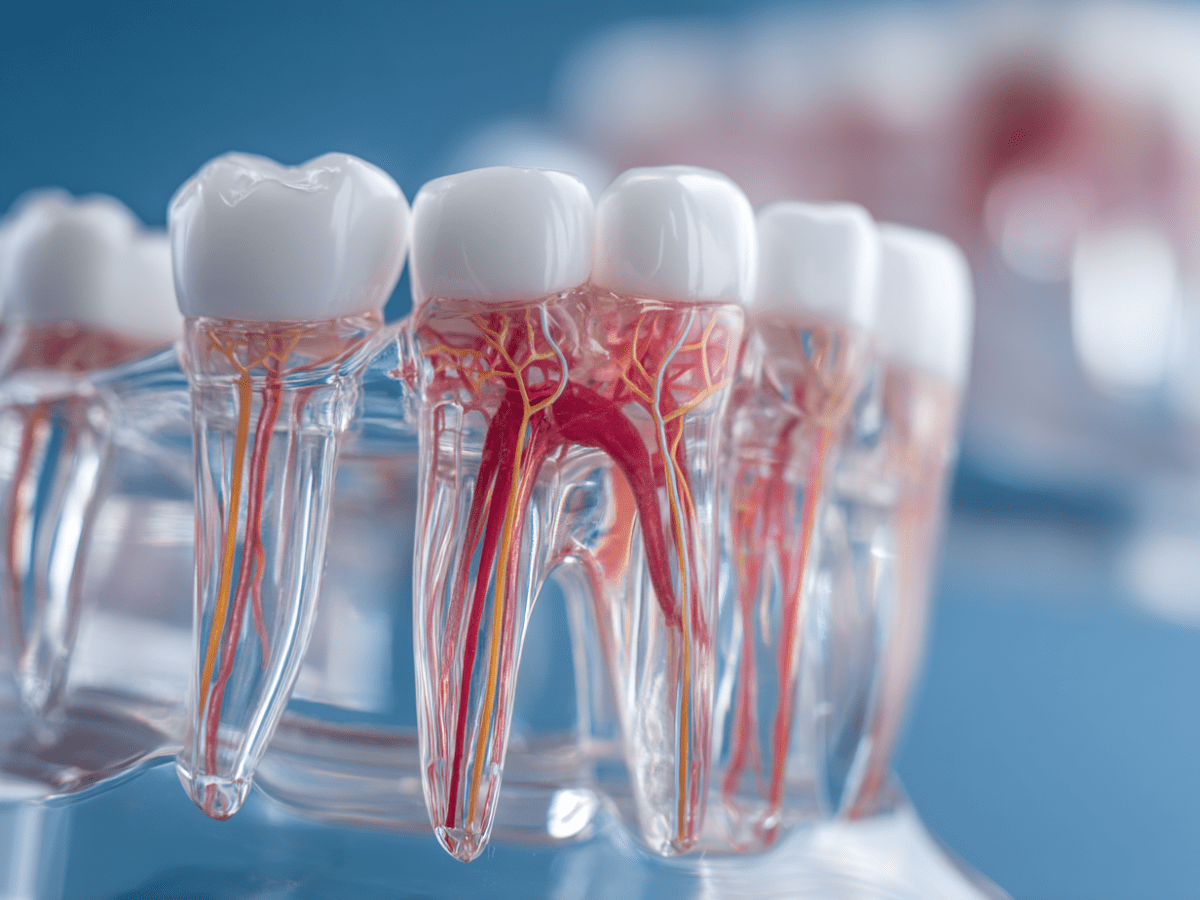
If the tooth can be saved, a root canal is typically recommended. This involves removing the infected dental pulp, disinfecting the space, and sealing it to prevent future infection. A restored tooth properly treated with a root canal can last for many years
Antibiotics

In cases where the infection has spread, or if the patient has a weakened immune system, your dentist may recommend antibiotics to prevent further bacterial growth.
Tooth Extraction
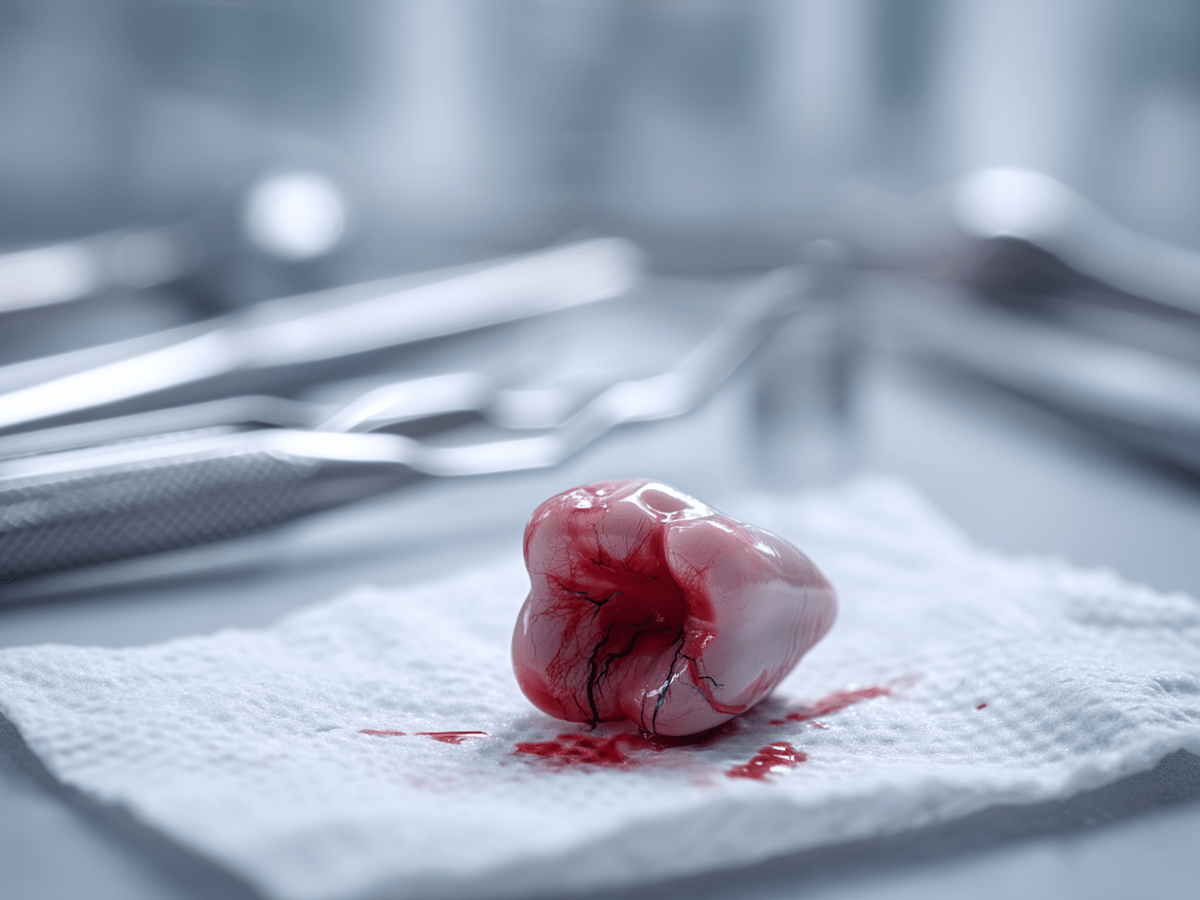
If the tooth is too damaged to preserve, it may need to be removed. Your dentist will recommend follow-up dental treatment, which may include implants or bridges to restore function and alignment.
At-Home Aftercare

During recovery, you may need to eat soft foods, avoid hot and cold temperatures, and brush with a soft toothbrush and fluoride toothpaste. Regular rinsing with warm saltwater helps reduce bacteria and inflammation..
Preventing Future Abscesses
Once you’ve recovered, keeping another abscess from forming starts with protecting your teeth and gums every day. Here’s how to reduce your risk and keep your smile healthy:
- Prioritize Daily Oral Hygiene: Brush twice a day with fluoride toothpaste and a soft toothbrush to remove plaque and bacteria. Don’t skip flossing, it helps clean along the gum line, where bacteria can easily collect.
- Stay Consistent With Dental Visits: See your dentist regularly for exams and cleanings. Early signs of a tooth infection or a failing restored tooth can be caught and treated before they become serious.
- Address Cavities and Cracks Promptly: Even a small cavity can give bacteria a way in. If a filling is loose or a crown is damaged, schedule dental treatment to restore the tooth properly before infection sets in.
- Eat and Drink With Care: Minimize sugary snacks and acidic drinks that feed bacteria and weaken enamel. Stick to a balanced diet, and drink water to keep your mouth hydrated and rinse away food particles.
Don’t Wait Until It Hurts: Your Smile Deserves Immediate Care
A tooth abscess isn’t something to monitor or manage at home, it’s a painful dental condition that requires timely care from a dental professional. Left untreated, it can lead to serious oral health issues, from tooth loss to life-threatening complications like the spread of infection to other parts of the body.
At Elizabeth L. Wakim DDS, we take your discomfort seriously. If you’re dealing with tooth pain, swelling in your face, or an unusual swollen bump near a tooth, our team is here to help. We offer compassionate, prompt care to help relieve pain, remove infection, and preserve your natural teeth whenever possible.
Call our Pennsylvania office at (724) 558-8222 or use our contact form to schedule a visit. Don’t let a small problem turn into a serious one, protect your smile today with expert, personalized treatment.

